|
SERVICES OFFERED
you are here: Home > SERVICES OFFERED > BARIATRIC SURGERY > DUODENAL SWTCHDUODENAL SWTCH
DUODENAL SWITCH 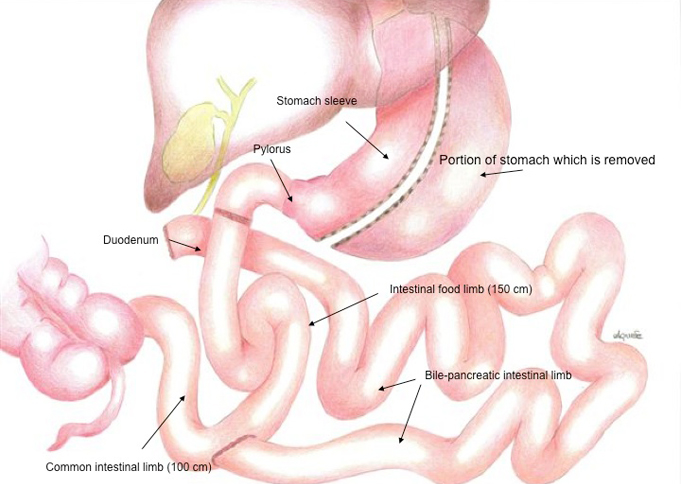 The Biliary Pancreatic Diversion (BPD) with Duodenal Switch (DS) is a procedure composed of a restrictive and a malabsorptive aspect. This variation was conceived to limit some of the side effects associated with BPD from which it differs in two fundamental ways:
1. Sleeve resection is performed leaving the pylorus intact (unlike with distal gastroresection)
2. The common limb is increased to 100 cm (as opposed to 50 cm)
This type of surgical operation was first carried out using laparoscopy by Michel Gagner in1999. After noting a high mortality rate and complications, Gagner introduced the “two stage technique” (i.e. technique involving two separate operations) for patients with a BMI>65. The first surgical procedure involves sleeve resection and only after significant weight loss has been achieved is the intestinal by-pass procedure carried out. In this way it has been possible to radically lower the mortality rate and reduce complications. Our centre has decided to limit this type of surgery to morbidly obese patients with a BMI of >60 only. We too have adopted the two-stage technique also because quite often the first surgical procedure (sleeve gastrectomy), which is quicker and less invasive, proves sufficiently effective to achieve the desired results in a large number of patients.
Advantages
- Preservation of the antropyloric region allows for normal vagal innervation and guarantees correct physiological gastric emptying with relative better absorption of many nutrients, especially calcium, iron and vitamin B12.
- Reduction in Dumping Syndrome
- Malabsorption, mainly lipidic, is brought about by diverting the bile and pancreatic juices so they meet the ingested food further down the digestive tract, i.e. the common limb, performed at a length of 100 cm.
- Less daily bowel movements, diarrhoea, vomiting and bone pain compared to BPD.
- Higher blood levels of ferritin, calcium and vitamin A compared to BPD.
- Effective control of type II diabetes (96%), hypertension and hypercholesterolemia.
Disadvantages
- long operating time
- the technique is complicated to master and requires a long learning curve
- symptoms of malabsorption may arise, such as diarrhoea and hypovitaminosis.
Complications
- haemorrhage and lesions to internal organs
- venous thrombosis and embolism: this is the formation of blood clots which may reach the lungs (pulmonary embolism). Pulmonary embolism is the main cause of post-operative mortality.
- Vomiting caused by the sudden reduction in stomach size and the onset of stenosis
- Respiratory insufficiency
- Gastric and/or intestinal fistula: opening of the stomach or intestine sutures. This complication may require corrective surgery or other medical treatments.
- Infection of the surgical wounds are more common in cases of open abdominal surgery.
- Intestinal occlusion caused by internal hernia or strangulated incisional hernia.
- The occurrence of post-operative complications may require additional and intensive medical treatment (e.g.: admittance to intensive care or reanimation ward) resulting in prolonged hospitalization for the patient. It is necessary to bear in mind that the risk of early post-operative mortality, which varies between 0.1% and 1% and of complications following surgery is higher the greater the body weight of the patient, his/her cardiorespiratory conditions and the experience of the surgeon. Smoking and alcohol abuse increase the likelihood of complications.
Results The recently held Consensus Conference on the DS operation illustrated the significant effectiveness of this procedure:
- long-term reduction of excess weigh at around 74% at 10 years of follow-up
- mortality rate 0 - 0.57%
- occurrence of gastric fistulas < 1%
- need for further surgery 3-5%
- incisional hernia in approximately 10%
- gastrojejunal anastomotic ulcer 8-10%
OSPEDALE REPUBBLICA DI SAN MARINO - ISS - VIA SCIALOJA, 20 - 47893 BORGO MAGGIORE - WWW.ISS.SM
|