SERVICES OFFERED
you are here:
Home > SERVICES OFFERED > BARIATRIC SURGERY > GASTRIC BANDINGGASTRIC BANDING
LAPAROSCOPIC GASTRIC BANDING (LGB)
LGB is a surgical operation of a restrictive type which together with other methods used in bariatric surgery has represented the technical solution most widely adopted over the last 20 years.
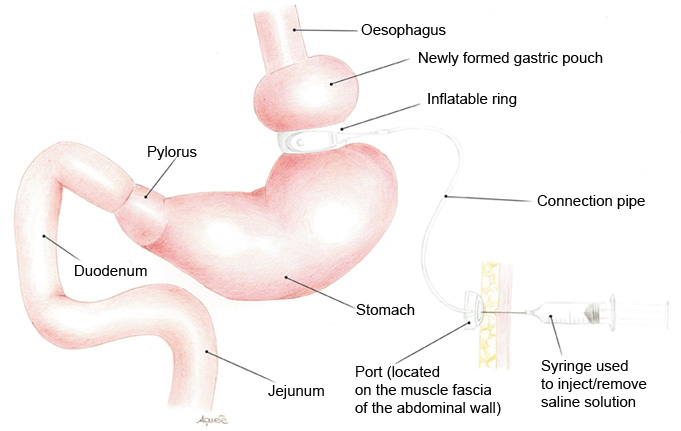
The operation entails creating a small pouch at the top of the stomach which communicates with the rest of the stomach by means of a tight orifice. The gastric pouch, with a volume of approximately 25 - 30 ml, is created by placing a silicone ring around the top of the stomach. A small tube connects the band to a port located above the muscle fascia of the abdomen wall. The port can be neither seen nor felt from the outside, except in some cases after weight loss. The ring is positioned around the stomach and has a special feature in that it can be inflated or deflated by a doctor. This operation is performed by simply adding or removing sterile saline solution to/from the port (these operations are performed through the skin) to alter the diameter of the connecting orifice.
Food eaten by the patient stretches the wall of the newly formed gastric pouch activating mechanoreceptors which stimulate the appetite centre on a hypothalamic level making the patient feel full. This surgical procedure is managed in outpatients. It is up to the medical team to give an indication as to when the band needs to be adjusted, based on multiple factors, not least the actual results in terms of weight loss.
This operation does not entail the removal or sectioning of organs and in anatomical and functional terms it is fully reversible. The procedure first described by Wilkinson in 1977 has undergone numerous changes, mainly in terms of the features characterizing the device. In 1992 Guy Bernard Cadiere, reproducing the open surgery technique demonstrated how gastric banding could be applied via laparoscopy.
The LGB represents the bariatric procedure of a restrictive nature most commonly performed in Europe and Australia. It was also approved by the Food & Drug Administration in 2001.
Limits of this technique depend on the type of diet followed by the patient. Obviously semi-liquid, high-calorie foods overcome the imposed restriction with ease and are readily absorbed. After the LGB has been positioned it is therefore essential for the patient to follow a suitable diet made up mainly of solid foods (proteins, carbohydrates and above all fibre).
Advantages
- Stomach restriction made using a gastric band does not involve structural modifications to the stomach.
- The band can easily be removed to restore the original shape of the stomach.
- The minimally-invasive procedure allows the patient to make a rapid post-operatory recovery with only a short stay in hospital required (usually 48 hours).
- The volume of the band is adjustable consequently the speed at which the stomach pouch is filled can be increased or reduced according to the individual’s needs.
Disadvantages
- This type of surgery can be totally ineffective if the patient does not follow an adequate dietary plan.
- Weight loss is less and slower compared to other procedures. Other bariatric surgery techniques are associated with greater risks and complications.
Complications
As well as general complications such as thrombophlebitis, pulmonary embolism, pneumonia, acute respiratory insufficiency, other complications may be:
- Intraoperative complications
- accidental perforation of the posterior stomach wall when the retrogastric tunnel is made (0.1% - 0.2%),
- bleeding following damage to the arterial vessels (branches of the left gastric artery, short vessels) or nearby organs (spleen and liver).
- Early post-operative complications
- acute “slippage” of the stomach with irreversible dilation of the gastric pouch (0.1% - 0.4%),
- premature intragastric penetration of the device ascribable to unrecognized perforation of the gastric wall which was not detected from post-operative radiological examination.
- Late post-operative complications
- dilatation of the gastric pouch (3 - 8%)
- intragastric migration (1 - 11%)
- infection of the port (0.4 - 2.2%)
- port displacement (0.4 %)
- leakage in the tubing connecting the port to the band (this risk is falling thanks to the innovative technology of the medical devices used).
The number of cases requiring further surgery as a result of complications fluctuates between 3.5 % and 15%. Management of patients with gastric erosion is controversial, in particular with regards timing and method of removal. Gastric erosion does not usually have to be solved urgently as the actual erosion process is slow and in most cases the patient shows no symptoms.
The mortality rate linked to surgery after 30 days is 0.15% (the same percentage as for laparoscopic cholecystectomy). No cases of medium- or long-term mortality have been reported.
With this operation an average 40 - 60% reduction in the pre-operative excess weight can be expected, with stable, long-term maintenance of weight loss in those patients who then follow an adequate diet and lifestyle.
Results
With gastric banding patients can expect to lose approximately 30% of their excess weight during the first 12 - 18 months following the operation. Studies on a European level have demonstrated that after the operation cooperative patients lose 49, 55 and 57 % of their excess weigh after 3, 4 and 5 years respectively.
After the operation for obesity patients maintain a high percentage of their weight loss over the following 10 years. Most of the medical problems associated with obesity (type 2 diabetes, high blood pressure, sleep apnoea, depression and back ache) improve or even disappear after the operation with lower percentages compared to other bariatric procedures.
Data provided in literature does not highlight any substantial differences between the laparotomic and laparoscopic methods in terms of morbidity and weight loss.