|
SERVICES OFFERED
you are here: Home > SERVICES OFFERED > BARIATRIC SURGERY > SLEEVESLEEVE
SLEEVE GASTRECTOMY 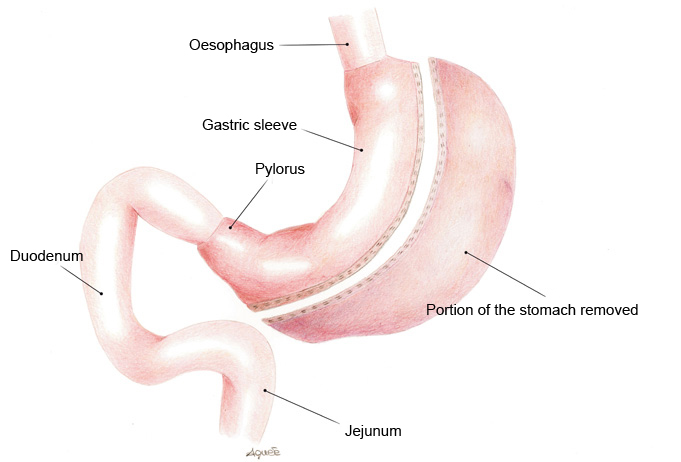 Laparoscopic Sleeve Gastrectomy (LSG) is a restrictive type of operation in which the stomach is surgically modified and shaped into a tube. LGS was originally developed in the United Kingdom and went on to be adopted in the United States, Germany and Belgium. The procedure, which can be performed laparoscopically, entails the removal of a large portion of the stomach which is excised using a special mechanical stapler. The remaining portion of the stomach is tubular in shape and has a drastically reduced volume with a capacity of approximately 100/150 ml. This procedure is not reversible in that a portion of the stomach is surgically removed. The stomach nerves and the pylorus (the stomach “outlet valve”) remain intact thus preserving stomach functions while the overall volume is reduced. When eating, food enters the tubular shaped stomach and fills it up by stacking, held only by the pylorus. Filling of the gastric sleeve determines a significant mechanical limit to the intake of further food and is accompanied by a feeling of satiety. Some studies have shown that the portion of stomach which is removed, especially the bottom part, produces ghrelin, one of the hormones responsible for causing a feeling of hunger. The reduction in the levels of this hormone after the operation leads to a reduction in appetite.
Loss of excess weight on average reaches 60% with results being maintained in the long term (depending on the cooperation of the patient).
In patients with a low BMI (35 - 45) the LGS procedure has been adopted as a single operation as it has proved to be efficacious when checked after 5 years.
This procedure could be of benefit to those patients with a low BMI (35 - 45) who suffer from anaemia or Crohn’s disease or have previously undergone extensive abdominal surgery or for those patients who need prolonged anti-inflammatory treatment as usually these types of medication have to be avoided after gastric by-pass operations. For patients with a high BMI (> 50 - 60) it is more difficult to perform a gastric by-pass or duodenal switch. Sleeve Gastrectomy can offer a reasonable solution to this problem as it provides efficacious initial weight loss. Once the BMI of the patient has dropped to an acceptable level, it is possible to perform a second surgical procedure which may be a gastric by-pass or a duodenal switch to obtain, whenever indicated, further weight loss. This bariatric surgical technique can be very quick and easy to perform, however unlike gastric banding this operation is not reversible and the long-term results are worthy of further study.
Advantages
- no foreign material is inserted in the body as with gastric banding operations
- the portion of the stomach responsible for producing the appetite-stimulating hormone, ghrelin, is removed.
- no Dumping Syndrome as the pylorus remains intact
- minimum risk of ulcer
- minimum risk of intestinal obstruction, anaemia, osteoporosis and protein and vitamin deficiencies
- highly effective as an initial procedure for patients with a very high BMI (> 50 - 60)
- good results as a single procedure for those patients with a low BM (35 - 45)
- surgical indication for patients with anaemia, Crohn’s disease and numerous other conditions which render gastric by-pass operations high-risk procedures
- it can be converted into another operation, such as a gastric by-pass.
Disadvantages
- as with all bariatric surgery procedures, initial weight loss may be followed by subsequent regaining of weight
- as with all restrictive type operations in those patients who consume liquid and high-calorie foods there may be a failure to lose weight
- the surgical operation is irreversible as part of the stomach is permanently removed.
Complications Complications are estimated at between 5% and 10%.
As well as general complications such as thrombophlebitis, pulmonary embolism, pneumonia, acute respiratory insufficiency, other complications may be:
- Intraoperative complications:
amongst these complications it is necessary to consider accidental perforation of the stomach wall, bleeding (1 - 3%) following lesions to arterial vessels (short vessels) or to adjacent organs (spleen and liver) or along the staple line.
- Early post-operative complications:
fistula along the staple line (2 - 5%) is a complication strictly linked to this type of procedure: in 80% of cases this is solved by intravenous feeding while waiting for the fistula to heal, in the remaining 20 % of cases another surgical procedure may be required.
- Late post-operative complications:
late gastric fistula is an event which may be associated with this procedure.
A gastric ulcer may also form penetrating the viscera wall. In general a surgical repair procedure is required.
The number of cases requiring further surgery as a result of complications fluctuates between 3.5 % and 25%.
The operation’s mortality rate after 30 days is 0.25%
Results Loss of excess weight after three years is between 50% - 80%. There is a possibility that the stomach will regain its original size resulting in a weight gain for the patient.
OSPEDALE REPUBBLICA DI SAN MARINO - ISS - VIA SCIALOJA, 20 - 47893 BORGO MAGGIORE - WWW.ISS.SM
|